Vitamin D, the Neglected and Forgotten Therapeutic Arsenal in the Fight against Covid-19
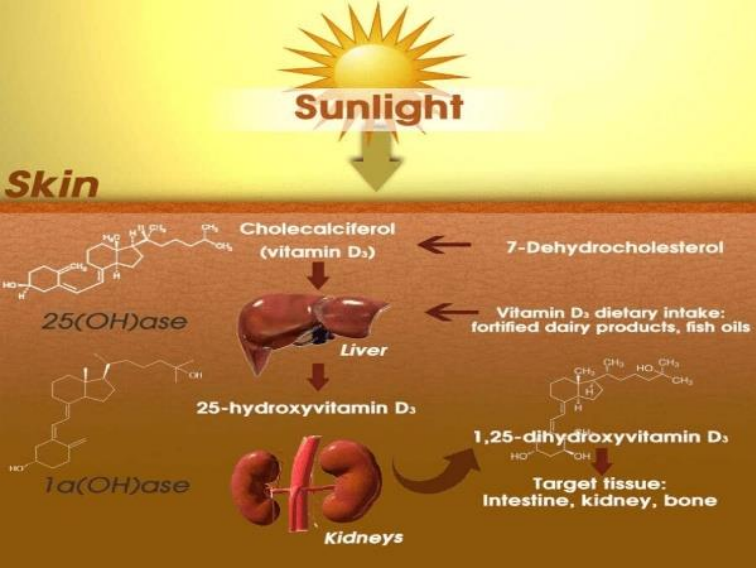
Vitamin D "sunshine vitamin" is a fat-soluble secosteroid provided by food and produced in
the form of vitamin D3 in the skin after exposure to ultraviolet rays (UVB), it is then
transformed into its active form in the liver and the kidneys. Vitamin D production starts from
acetyl-CoA following the cholesterol production pathway until 7-dehydrocholesterol is
synthesized. Statins act through the reversible block of hydroxy-3-methylglutaryl-coenzyme
A reductase (HMG-CoAR), thereby reducing cholesterol synthesis and the production of 7-
dehydrocholesterol and vitamin D. Statins do not prevent your body from absorbing
cholesterol from your food, but instead prevent your liver from making it by blocking an
enzyme in the mevalonate pathway called HMG-CoA reductase, which is used to make
cholesterol in the liver. Cholesterol is found in almost every cell in your body. This waxy
substance is vital for optimal functioning of cell membranes, regulation of protein pathways,
and support of brain health, hormone levels, and reduction of heart disease risk. Image 1
The increased emphasis on protecting the skin against sun damage (fear of cancer) and the
shift from an outdoor to an indoor and restricted lifestyle in recent generations has led to a
serious vitamin D deficiency problem in many developed parts of the world. Added to this are
recommendations to limit the consumption of animal fat wrongly accused of the emergence of
cardiovascular diseases.
Vitamin D deficiency is a global public health problem in developed and developing countries.
Low levels of vitamin D are associated with upper and lower respiratory tract infections, heart
disease, asthma, cancers, diabetes, multiple sclerosis, HIV, hypertension, inflammatory
diseases of the intestine, Alzheimer's disease and other autoimmune diseases.
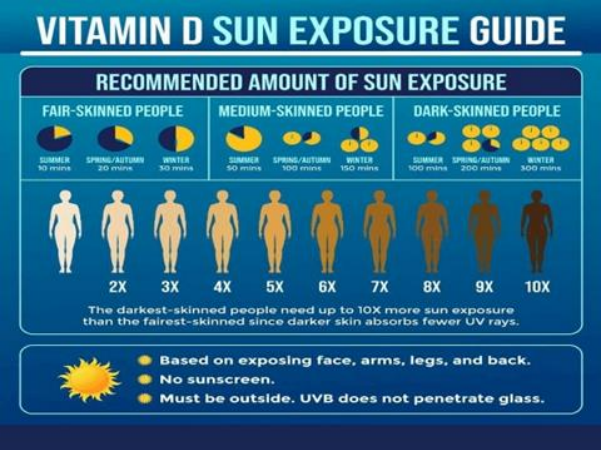
People with naturally dark skin tones benefit from natural sun protection and require at least
three to five times longer exposure to produce the same amount of vitamin D as someone with fair skin tones. Image 2
Vitamin D being fat soluble can be stored in fatty tissues. Accordingly, experimental and
human studies suggest that greater storage of vitamin D in body fat decreases its
bioavailability, hence the need for obese people to dissolve their body fat stores by fasting or
exercising to benefit from it.
Vitamin D deficiency has been found to contribute to acute respiratory distress syndrome;
and…case fatality rates increase with age and with comorbidity of chronic diseases, both of
which are associated with lower 25(OH)D concentration.
Vitamin D supplementation causes at least 1.5-fold change in expression of genes involved in
apoptosis, immune function, transcriptional regulation, epigenetic modification, stress
response, cell cycle activity and differentiation. This finding is consistent with previous in
vitro studies which have shown that 1,25(OH)2D3 directly or indirectly controls more than
200 genes, including genes responsible for regulating cell proliferation, differentiation,
angiogenesis and immunomodulatory activities on innate and adaptive immune responses.
Researchers have shown that vitamin D has a "significant protective effect" and reduces the
risk of acute respiratory infection from 60% to 32% of patients as well as it may help prevent
respiratory infections and reduce the use of antibiotics.
According to research done by GrassrootsHealth's group of 48 vitamin D researchers, 40
ng/ml is the lower edge of the optimum, with 60 ng/ml to 80 ng/ml being ideal for health
and disease prevention.
There is strong scientific evidence that vitamin D plays a central role in your immune
response and your ability to fight infections. Recent studies supporting higher vitamin D
levels may lower your risk against COVID-19 and its complications.
Mounting evidence suggests that your vitamin D status may also play an important role in the
development of COVID-19, as well as the severity of the disease.
Vitamin D plays an important role in reducing the risk of respiratory tract infections,
knowledge about the epidemiology of influenza and COVID-19, and how vitamin D
supplementation might be a useful measure to reduce the risk. Through several mechanisms,
vitamin D can reduce the risk of infections.
These mechanisms include the induction of cathelicidins and defensins which can lower viral
replication rates and the reduction of proinflammatory cytokine levels which produce the
inflammation that damages the lining of the lungs, leading to pneumonia, as well as the
increase in concentrations of anti-inflammatory cytokines…
Evidence supporting the role of vitamin D in reducing the risk of COVID-19 includes that the
outbreak occurred in winter, when 25-hydroxyvitamin D (25(OH)D) concentrations are the
weaker; that the number of cases in the southern hemisphere towards the end of the summer is
low.
Diabetic patients with liver or kidney problems are at high risk of deficiency, as are patients
with gastrointestinal disorders such as celiac disease, pancreatitis, low bile levels, thus
worsening their health status with respect to live with Covid-19.
There are many things we can do to improve our resistance to infections. These include
getting regular physical activity, enjoying a healthy diet and getting plenty of sun exposure to
replenish vitamin D, getting enough sleep, and quitting smoking. Taking multivitamin
combinations that include vitamin D, or a vitamin D supplement, probably can't hurt, and it
might help. Image 3
One thing to keep in mind is that our bodies can store vitamin D in liver and fatty tissue, so
there are plenty of opportunities to make vitamin D in the spring and summer. Preparing for
winter with a good reserve of vitamin D remains as vital as necessary to possibly help our
immunity to face the threats of covid-19 just in case?